It’s September! There is a fresh school year beginning for some and others are embarking on the beginnings of their career as new grad clinicians.
Five years ago, I had just begun my PT residency in a private practice. I was like a massive sponge, wanting to absorb all of the knowledge I could and registered for every course I could right away during my first year. Looking back I wouldn’t recommend this approach to new therapists. Instead, I wish I had taken things in stride, slowed down a bit more to enjoy my new career. One thing I did realize in doing all of this, was what really interested me. I wanted to learn more about how the brain and sensory systems integrated to control movement, particularly in athletes. At the time, concussion rehabilitation was growing incredibly popular as this new, exciting area of physiotherapy. Finding the common ground between my interests in “neurosport” science and a growing field of rehabilitation led me to taking on a PhD to try and answer my own clinical questions. The academic route isn’t for every clinician, but if you’re eager to learn about concussion rehabilitation as a new grad there are a number of other ways to do it.
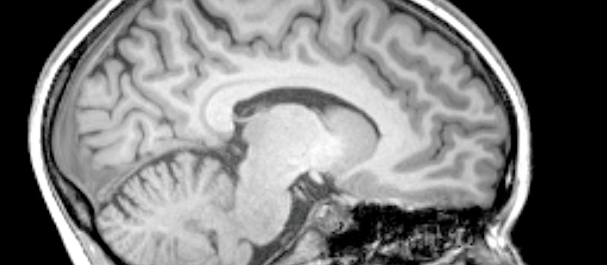
Concussion has been a scary dimension of clinical care for some; let’s face it, the brain is complicated. With endless connections and synapses between billions of neurons, to this day there are still several neural pathway and networks yet to be discovered. Not only that, but each individual brain is different, it is shaped by our experiences, abilities, and several other factors, including injury and disease. The more time I spend studying it, the more complicated it seems to be!
As a new clinician, this is a lot to absorb. The big question is, how does a new practitioner become confident in assessing and managing patients with concussion?
Unfortunately, the answer isn’t black and white (the brain is comprised of a lot of gray [matter]!). Taking an introductory course can be a great starting point to outline the basics. There are a handful of good courses in Canada that are provided by credible instructors that I would highly recommend. Even so, these instructors would emphasize that the complexity of this area requires more time invested than a weekend or two.
My recommendations for a new clinician interested in improving and progressing their skills in concussion management are the following,
1. Don’t forget about the basics you learned in neuroanatomy & rehab courses!
As a new grad, you are full of fundamental knowledge about the brain and neuromuscular system. Learning to apply that knowledge is key to becoming a good practitioner. Refer back to the basics of neuroanatomy, physiology, and motor control, and use this knowledge to help understand the concussion literature and to educate your patients.
2. READ the literature.
This is one of the key skills that are now being taught in allied health programs. New grads are well-equipped with the skills to critically appraise academic literature. The best part about this is that a lot of the primary concussion literature is OPEN access. Yes, these resources are free. Check out the references with links below for some key articles!
3. Find a mentor that can guide you through practical learning.
Mentorship can be unbelievably helpful in various scopes of practice, concussion care being one of them. Having a good mentor who specializes in evidence-based concussion rehabilitation can help answer questions and provide practical scenarios. Working with another therapist prior to taking on your own patients can help build confidence and understanding of best practices aligned with the current international recommendations.
4. TIME
Just like any skill development, becoming a stronger practitioner in concussion will take some time (a lot of it!). I’ve spent years engulfed in research and clinical practice, and I learn new things all of the time. Each individual patient will be different. If you have a solid foundation of knowledge and practical skills then the only way to continue to progress is to practice!
An additional recommendation is to connect yourself with an inter-disciplinary network for appropriate referrals when things go beyond your skill set and/or scope of practice. There is nothing wrong with having someone you can refer to when you don’t feel that your skill set will benefit the patient’s recovery. We cannot help every single person that walks into the clinic. Understanding how to screen and identify dysfunction of any one of the clinical domains of concussion can help guide your patient on the right path, even if it’s not with you. A concussion is so multi-faceted, that having a referral network follows best practices to achieve optimal outcomes!
Some key concussion research articles and practice recommendations!
McCrory, P., Meeuwisse, W., Dvorak, J., Aubry, M., Bailes, J., Broglio, S., … & Davis, G. A. (2017). Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med, 51(11), 838-847.
https://bjsm.bmj.com/content/bjsports/early/2017/04/26/bjsports-2017-097699.full.pdf
Leddy, J. J., Haider, M. N., Ellis, M., & Willer, B. S. (2018). Exercise is medicine for concussion. Current sports medicine reports, 17(8), 262-270.
https://europepmc.org/articles/pmc6089233
Schneider, K. J., Leddy, J. J., Guskiewicz, K. M., Seifert, T., McCrea, M., Silverberg, N. D., … & Makdissi, M. (2017). Rest and treatment/rehabilitation following sport-related concussion: a systematic review. Br J Sports Med, 51(12), 930-934.
https://pdfs.semanticscholar.org/76e1/f34fcba71b9842f440c6f0984ab3f2a7abaf.pdf
Echemendia, R. J., Meeuwisse, W., McCrory, P., Davis, G. A., Putukian, M., Leddy, J., … & Schneider, K. (2017). The sport concussion assessment tool 5th edition (SCAT5): background and rationale. Br J Sports Med, 51(11), 848-850.
https://bjsm.bmj.com/content/51/11/848.abstract
Moran, R. N., Covassin, T., Elbin, R. J., Gould, D., & Nogle, S. (2018). Reliability and normative reference values for the Vestibular/Ocular Motor Screening (VOMS) tool in youth athletes. The American journal of sports medicine, 46(6), 1475-1480.
Ellis, M. J., Cordingley, D., Vis, S., Reimer, K., Leiter, J., & Russell, K. (2015). Vestibulo-ocular dysfunction in pediatric sports-related concussion. Journal of Neurosurgery: Pediatrics, 16(3), 248-255.